Diaphragmatic Hernia Surgery
Dogs
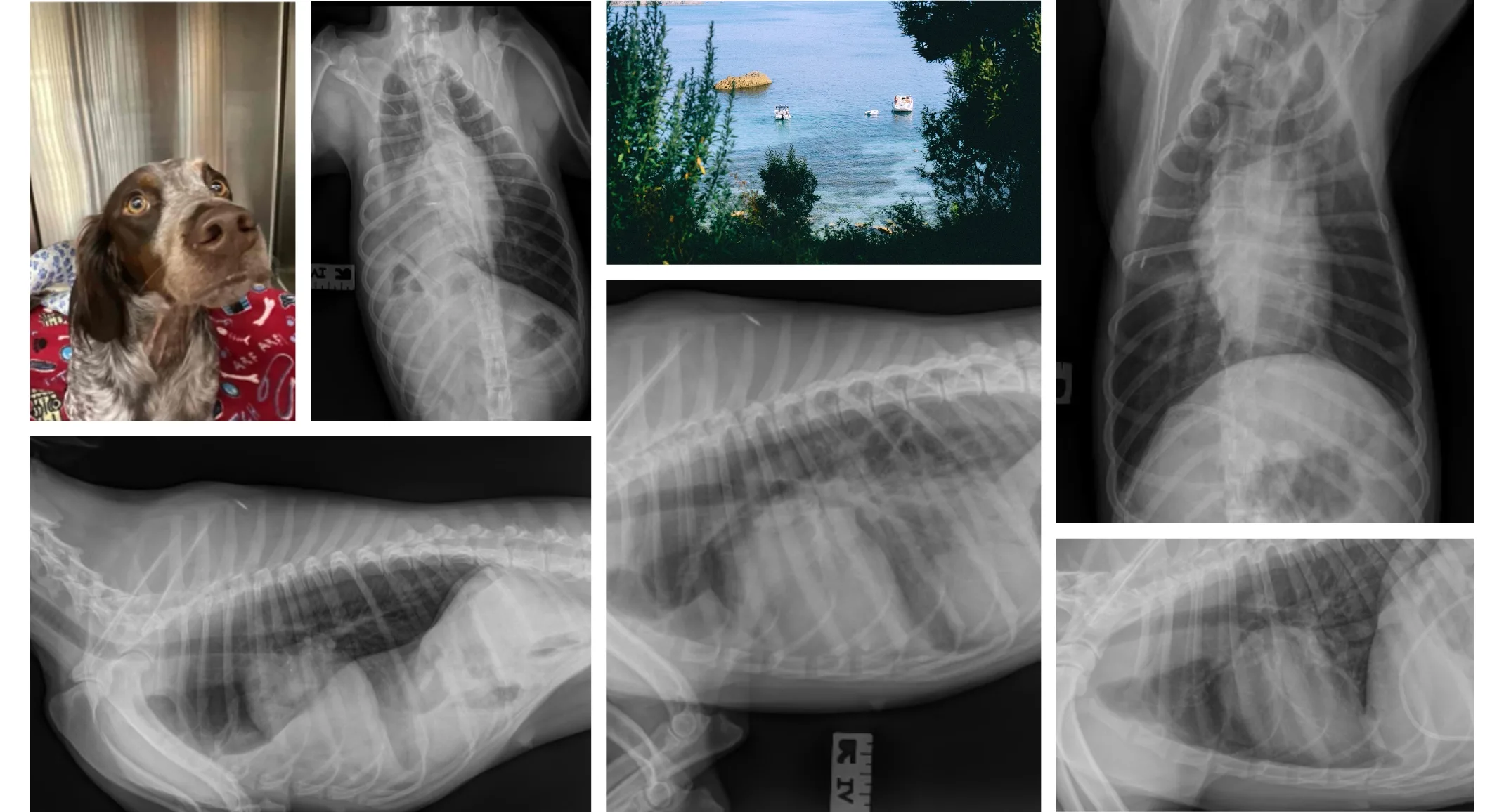
Marilyn is a 1.6-year-old Female Brittney Spaniel. She presented to an emergency veterinary clinic after being hit by a car. She had superficial wounds on her rear limbs. She was observed overnight without complications. The next day she was sedated for treatment of her wounds. During sedation, she developed anesthetic complications. She recovered from sedation with supportive care. Radiographs were performed.
A diaphragmatic hernia was revealed. The patient was referred to VSB emergency service for diagnostics and treatment. On admission to the emergency service, Marilyn was bright, alert, and responsive. She did not exhibit overt symptoms but did have decreased lung sounds on auscultation of the right hemithorax. A full assessment revealed that she had an ALT >1300 U/L and was suffering from preventricular contractions. She had obviously sustained severe trauma to the abdomen and thorax. She was treated for 24 hours with supportive care and the VPC’s resolved.
Marilyn was transferred to the surgical service for surgical consultation. Approximately 15% of patients with diaphragmatic hernias die before treatment. Marilyn was beyond this complication period. Historically there was an approximately 50% mortality rate with surgical treatment of diaphragmatic hernias. These deaths often occurred when patients were taken to surgery within 12 to 24 hours of admission/trauma. Because Marilyn was stable, her surgery was scheduled beyond the 72-hour recommended waiting period. This also gave Marilyn a chance to further recover from her arrhythmia and liver trauma.
Marilyn returned for surgery 4 days later. She remained clinically asymptomatic. Her arrhythmia remained resolved and her ALT decreased to 257 U/L. Marilyn was prepped and clipped before induction to facilitate quick surgical intervention. Upon induction, Marilyn quickly developed hypotension and hypoxia. An expedited celiotomy revealed a large right-sided diaphragmatic hernia. The hernia contained the liver, gallbladder, duodenum, and part of the jejunum. The right lung fields were completely compressed by the herniated organs when placed in dorsal recumbency. The abdominal viscera were reduced to the proper location. Her condition stabilized. A large radial tear of the diaphragm was found that extended from the dorsal body wall to the sternum.
The viscera were retracted allowing reconstruction of the diaphragm. The diaphragmatic tear originated in the right crus and transversed adjacent to the esophageal hiatus and caval foramen before terminating in the pars sternalis. Respiration was controlled with a ventilator while the diaphragm was carefully sutured. Because the diaphragm avulsed from the esophagus and cava tedious suturing was necessary. A thoracostomy tube was placed for controlled reinflation of the lungs. No complications occurred during the surgery. Marilyn recovered with supplemental oxygen. Controlled evacuation of the pneumothorax helped prevent re-inflation injury. Vital parameters remained stable. The thoracostomy tube was removed the following day. Radiographs confirmed normal thorax.
